Introduction: A unique subgroup of AML is defined by the presence of the TP53 mutation, with worse overall survival (OS) and limited therapeutic options (Döhner et al, Blood 2022; Daver et al, J Hematol Oncol 2023). Clinical trials are essential for establishing the efficacy and safety of new treatment options in AML; yet, they may not be generalizable to patients with TP53 mutation, who are often older adults with comorbidities and prior treatment exposure. Thus, the optimal treatment for TP53 mutated AML is unclear. Real-world data (RWD) can provide insights into demographic and clinical characteristics, as well as the utilization, effectiveness, and safety of treatment regimens used in routine clinical practice. This RWD study aimed to describe the characteristics, first line treatment patterns, and outcomes in patients with ND-AML with TP53 mutation in a real-world cohort of adult patients in the US.
Methods: A retrospective observational study was conducted using the COTA real-world database, a de-identified source of longitudinal electronic health record (EHR) data pertaining to the diagnosis, clinical management, and outcomes of patients with cancer. The study population included adult patients (≥ 18 years) with ND-AML and confirmed TP53 mutation status (positive or negative) per Next-Generation Sequencing (NGS), who were diagnosed between January 1, 2013, and March 20, 2023. Patients were excluded if key study data were missing (i.e., if TP53 mutation status was unknown, or if the testing methodology was unspecified), or if an AML-defining recurrent genetic abnormality superseded TP53 in the hierarchical classification of the International Consensus Classification. First-line treatment regimens were mapped to relevant therapeutic categories (e.g., intensive chemo [IC] with cytarabine, hypomethylating agent with venetoclax [HMA+ven]) and summarized across clinical and demographic patient characteristics using descriptive analyses.
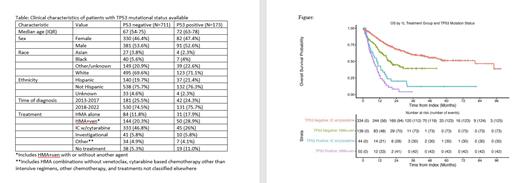
Results: A total of 884 patients ND-AML with analysis of TP53 status were identified, including 173 TP53 positive (TP53+) and 711 negative (TP53-). Patients who were TP53+ were older, and otherwise demographically similar to those who were TP53- (see table). Testing for TP53 increased over time, with about 75% of tested patients being diagnosed in 2018-2022 versus 25% in 2013-17. All patients who were TP53+ were by definition ELN adverse risk group, whereas 36.8% of patients with TP53- AML were adverse risk. The most commonly used treatment regimens included hypomethylating agent (HMA) alone (17.9% of TP53+ and 11.8% of TP53-), HMA with venetoclax (HMA+ven) (28.9% TP53+, 20.3% TP53-), and IC w/cytarabine (26% TP53+, 46.8% TP53-). Patients with TP53+ AML were more likely to not receive any anti-leukemic treatment. Patients with TP53+ AML were less likely to achieve complete remission (CR) compared to those with TP53- AML (31.2% versus 46.1%, excluding patients in each subgroup who did not receive anti-leukemic treatment). In this cohort, OS was shorter for patients with TP53+ AML compared with those with TP53- AML. This difference was seen consistently in patients treated with the two most common regimens (IC w/cytarabine and HMA+ven) (Figure). OS appeared longer for patients treated with IC w/cytarabine in patients with or without TP53 mutation, but it should be noted that these patients were younger and generally more fit than patients receiving HMA+ven (61 years versus 75 years among patients with TP53+ AML).
Conclusions: In patients with TP53+ AML, CR and OS are lower overall and when specific treatment options are compared to patients with TP53- AML. This difference was seen in patients receiving either of the two most commonly used treatment regimens. This study demonstrates the capability of using RWD to characterize the outcomes of a specific genetic subtype of ND-AML despite widespread testing for this marker only occurring in the latter half of the study timeframe. These findings are subject to the inherent limitations associated with observational data, including the challenges in collecting and analyzing real-world data (e.g., missing treatment data or other characteristics) which may result in bias or limited generalizability of study findings. Finally, this study further demonstrates that research into novel treatment of TP53+ AML is needed to improve patient outcomes.
Disclosures
Fernandes:COTA: Current Employment. Wynne:Carisma Therapeutics: Patents & Royalties: Patents related to HIV therapy. Hansen:COTA: Current Employment, Current equity holder in private company. Belli:COTA: Current Employment, Current equity holder in private company. Barcellos:COTA: Current Employment. Zettler:C OTA: Current Employment. Wang:COTA: Current Employment, Current equity holder in private company.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal